LATEST ON COVID-19
Apr27 2020 |
The Employer Will Test You Now - WSJ → Read more |
Apr27 2020 |
“Suppress and lift’: Hong Kong and Singapore say they have a coronavirus strategy that works | Science | AAAS → Read more |
Apr27 2020 |
Mandated Bacillus Calmette-Guérin (BCG) vaccination predicts flattened curves for the spread of COVID-19 | medRxiv → Read more |
Apr25 2020 |
Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19 Infection → Read more |
Apr25 2020 |
The NATIONAL COMPREHENSIVE #COVID19 MANAGEMENT HANDBOOK for Ethiopia has been published for the effort to contain the epidemic and guide policymakers, healthcare providers and public heath professionals at all levels. → Read more |
Apr25 2020 |
WHO looks into report of Covid patients testing positive after negative tests → Read more |
Apr25 2020 |
COVID-19 pneumonia: different respiratory treatment for different phenotypes? → Read more |
Apr25 2020 |
The Preparedness Problem — how America spent 20 years getting ready to fight a pandemic, and then dropped the ball when it finally arrived. → Read more |
Apr25 2020 |
Data on 53 Patients Treated With Investigational Antiviral Remdesivir Through the Compassionate Use Program Published in New England Journal of Medicine → Read more |
Apr25 2020 |
Important papers on aerosol transmission of SARS-CoV-2 → Read more |
Apr25 2020 |
Compassionate Use of Remdesivir for Patients with Severe Covid-19 | NEJM → Read more |
Apr25 2020 |
Jigjiga University will inaugurate it's COVIDー19 Molecular Diagnostic Centre April 11. The center will have a capacity to test of 240 samples per day. → Read more |
Apr25 2020 |
How COVID-19 invaded my house and my family → Read more |
Apr25 2020 |
A New Normal With COVID-19: The Next Steps We Must Take | Think Global Health by Tom Friedan, MD, MPH (former head of CDC) → Read more |
Apr25 2020 |
Face masks for the public during the covid-19 crisis → Read more |
WHO looks into report of Covid patients testing positive after negative tests
WHO looks into report of Covid patients testing positive after negative tests
The World Health Organization (WHO) has said it is looking into reports of some Covid-19 patients testing positive again after initially testing negative for the disease while being considered for discharge.
On Friday South Korean officials reported that 91 patients thought to have been cleared of the new coronavirus had tested positive again. Jeong Eun-kyeong, the director of the Korea Centers for Disease Control and Prevention, told a briefing that the virus may have been “reactivated” rather than the patients being re-infected.
Jigjiga University will inaugurate it's COVIDー19 Molecular Diagnostic Centre April 11. The center will have a capacity to test of 240 samples per day.

How COVID-19 invaded my house and my family
How COVID-19 invaded my house and my family
I am an ER doctor, and my husband is a pediatrician. This story starts two weeks ago when COVID-19 was first changing all our lives. I am a travel doctor and was returning home. I saw a few patients that I was sure had COVID-19 (later confirmed). Fortunately, I worked in one of the rare ERs that had enough PPE, and I had worn it with each of those patients, so I wasn’t too worried. Little did I know what was coming.
Returning home Sunday afternoon, exhausted after working 7 of 8 days, I worried about bringing COVID-19 into our home. Neither of us had active symptoms, but we decided to sleep in separate rooms and use separate bathrooms for two weeks until my possible incubation period ended. This proved to be a crucial decision that kept one of us well. Monday morning, my husband went to work feeling fine, but by that evening was achy and could barely keep his eyes open. By Tuesday morning, he was clearly ill, sleeping all day and suffering from body aches when he woke. There was still no fever or cough. When I checked on him that night, he asked if one of his calves felt cold. He had paresthesias, a sensation he also described as an ice cube in the middle of his back. The next morning, an article came out about a local nurse with similar symptoms that had tested positive for COVID-19. We decided he needed a test for COVID-19, and the health department agreed. He hasn’t left our house since that day.
I had already initiated the second phase of strict home infection control/quarantine on Tuesday. I wore a mask and gloves every time I went into the “hot zone” (our bedroom/his prison), used bleach solution daily on common surfaces/doorknobs, and ran the dishwasher/washing machine on sanitize. For the next several days, my husband continued suffering from body aches and debilitating fatigue. I took him meals and fluids (while masked and gloved), but otherwise, we lived separately in the same house. COVID-19 was confirmed Saturday, three days after his test. That was eight days after his “prodrome,” 3 hours of cough and aches he remembered from 2 days before I came home. The next day, day 10, he seemed to be improving, making it outside for a few minutes and holding a short conversation! We had our first scare a few hours later.
That night, I woke to knocking on my bedroom door. My husband stood there, masked and gloved, saying he couldn’t breathe. His breathing was fast and labored with an oxygen saturation of 88 percent (98 percent or above is normal). His lungs sounded clear, but he wasn’t moving enough air. As doctors, we weren’t going to the ER unless I felt he couldn’t breathe without support, so I started thinking about how to open his lungs and remembered the incentive spirometer (IS), a device that encourages slow deep breaths to force in more air. I got in touch with a nurse practitioner friend and monitored him closely overnight. My friend left the IS at our door several hours later. We managed to stay out of the ER. Now he is making improvements but still gets short of breath talking or with even small amounts of activity. There have been several repeated scares when he was struggling to breathe, and I almost took him to the ER. He is a young, healthy person. Day 15 and quarantine continues.
I never imagined COVID-19 would enter our house this way. My job is much more “high risk” for exposure. My husband did not have any definite sick contacts, and he had not traveled. He got sick before community spread was confirmed in our area. Dealing with the threat of this virus at work and now in my home has been a double whammy. I have not been able to hug, kiss, or even touch my husband in almost two weeks. I wear gloves and mask just to look in at him. I think about every move I make, every object, surface, and doorknob in our house that must be cleaned daily. I can’t even have a conversation with him because he gets short of breath after a couple of minutes. Every day is lonely, even though I’m not alone. Every day I remain healthy and without symptoms is a victory. You do not want this invisible enemy in your home. You do not want to watch someone you love struggling to breathe, wondering if they will end up hospitalized on a ventilator, dying scared and alone. With Easter fast approaching, my fear as a physician is that those who don’t know anyone that has been infected will think it’s OK if “just their family” has a traditional family dinner, or “just a few families” have an Easter egg hunt. That would undo all our social distancing efforts and the curve we have all worked so hard to flatten. It would bring New York’s nightmare into our own towns.
Soon I will be clear from quarantine and back in the ER. I don’t want to stand, covered head to toe in PPE, over your terrified loved one telling them we must sedate them, paralyze them, and insert a breathing tube. Put yourself there: it must be the worst kind of fear, lying helpless and alone on a cold, hard stretcher struggling for air. I don’t want to pronounce your loved one dead after our valiant efforts fail. My plea is for all to maintain social distancing, stay home, and avoid the ER unless it’s necessary. It is working, but we must keep up the fight. I have practiced emergency medicine over a decade, and we never have as health care professionals asked the public for anything. Well, now we are asking, and your choices as a person, as a community, city, and state matter. It is quite literally life and death.
Raina L. Shanks is an emergency physician.
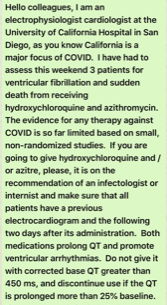
Unnecessary risk of a major public health hazard with chloroquine publicity.
From Sanjay Gupta
Clinical Presentation
Symptoms and Labs/Imaging
initial analysis from the outbreak in China (n=44,000)
The majority of infections were in 30-70 year olds
Disease Severity – 1.2% asymptomatic, 80% mild 20% severe disease (testing started after outbreak and may underestimate asymptomatic)
Symptoms:
• Fever 43.8%(eventually in 80%)
• Cough 67.8% (Sputum 33.7%)
• Fatigue 38.1%
• Shortness of Breath 18.7%
• Myalgia/Arthralgia 14.9%
• Sore throat 13.9%
• Headache 13.4% v
Lab/imaging:
• Lymphocytopenia (<1500) 83.2%
• CRP > 10 60.7%
• CXR abnormality 59% (most commonly bilateral or local patchy shadowing)
Other reported Symptoms
• Reports of anosmia in as high as 30-50% of patients (anecdotal reports) 3/23/20
In a small study while diarrhea and sinusitis were seen all patients with those symptoms also had cough however one patient had just rhinitis and otitis with no other symptoms
Cough 7/9, Fever 2/9, Diarrhea (2/9 both had cough and fever) , sinusitis 4/9 (all had cough), rhinitis (2/9, 1 also with otitis 1 with cough), Asymptomatic 1/9 (n=9 Germany)
3/15/20 possible signal that diarrhea may be more common than previously thought in presentation
Chloroquine for Treatment of COVID19 from Geoff Modest
A systematic review of the efficacy and safety of chloroquine (see covid Chloroquine reviewjcitcare2020in dropbox, or doi.org/10.1016/j.jcrc.2020.03.005)
Details:
— 6 articles were reviewed (one letter, one in-vitro study, one editorial, one expert consensus paper, and 2 national guideline documents)
— there are 23 ongoing clinical trials in China using chloroquine or hydroxychloroquine in different groups and looking at different outcomes: patients with mild to severe to critically ill Covid-19, with outcomes including conversion to a negative PCR assay, normalizing clinical symptoms, clinical recovery time, length of hospital stay, mortality rate, etc. A few studies are comparing it to lopinavir/ritonavir
Results:
— one Chinese lab study found that of 7 antivirals tested, remdesivir and chloroquine were remarkably effective in suppressing SARS-CoV-2, even at quite low doses. chloroquine, unlike remdesivir, functioned at blocking both SARS-CoV-2 cell entry as well as at the post-entry stages of infection, remdesivir only the latter (see covid Chloroquine reviewjcitcare2020 in dropbox, or Wang M. Cell Research 2020; 30: 269), and chloroquine has good penetration into lung tissue
— another article found that in more than 100 patients chloroquine inhibited the exacerbation of pneumonia, improved lung imaging findings, promoted a virus conversion to negative, and shortened the disease course. I should add that the above systematic review of chloroquine did not find evidence of such data in their trial registries
— a Chinese multi-collaborative expert consensus concluded that chloroquine 500 mg twice a day for 10 days was recommended for people with mild, moderate, and severe cases of SARS-CoV-2 pneumonia. They also suggested blood testing to rule out the development of anemia, thrombocytopenia, or leukopenia as well as electrolyte disturbances or hepatic/renal dysfunction, and an EKG to rule out development of QTc prolongation. Of note, this consensus document was relying on information that has not yet been published
— the Dutch Center of Disease Control suggested administering chloroquine to treat severe infections requiring admission to the hospital and oxygen therapy or admitted to the ICU, though treating with optimal supportive care was also considered a reasonable option
— the Italian Society of Infectious and Tropical Disease recommended the use of chloroquine or hydroxychloroquine for 5 to 20 days according to the clinical disease severity, but including those with mild respiratory symptoms who had comorbidities
Title of articles
Modal Description
Title of articles

Modal Description
BAIREX INTRODUCES THE BROAD STROKES ™ MEDICAL EDUCATION LECTURE SERIES
Bairex’s medical education lecture series called Broad Strokes ™ incorporates key aspects of both national and international conferences which occur throughout the year.
One of our current main areas of interest in Africa and the Middle East is non-communicable diseases (NCDs). NCDs are emerging as the leading cause of illness and death worldwide, especially in the low and middle income countries. This shift towards NCDs in developing countries has dispelled the popular myth that NCDs primarily afflict affluent (high income) populations. Many LMICs, are currently undergoing epidemiological transitions from predominantly infectious diseases to NCDs. This change can be attributed to changing lifestyles that promote western diet and physical inactivity. Current projections show that the largest increases in NCD deaths by 2025 will be in LMICs.
Therefore, our current emphasis is to educate about NCDs, including:
- Cardiovascular diseases
- Oncology & hematology
- Respiratory diseases
- Metabolic diseases: diabetes
- Neurodegenerative diseases
Our educational objectives are multifold. We aspire that our expert faculty highlight the magnitude of and socio-economic impact of particular NCDs in Africa and the Middle East, identifying the primary risk factors, primary prevention of the NCD and early treatment. The Pan-African and Middle Eastern experience of evolving NCD prevention/control and testing recommendations as well as current management practices should be addressed. Emphasis should be placed on the approaches underway by various nations and communities to strengthen local, country and global initiatives to prevent and control NCDs as part of national health plans and sustainable development frameworks.
Our mission is to share knowledge and create forum for collaboration with fellow medical doctors, nurses, pharmacists and other health care professionals
To Stop the Sale of Falsified Medicines, Africa Must Free Itself from Dependence on Foreign Drugmakers
By Dr. Menghis Bairu
A few years ago I travelled to Ghana to see the state-of-the art pharmaceutical research and manufacturing company a friend had established there. He had long worked as an executive for several of the largest pharmaceutical companies in the United States before launching his company with the goal of bringing to Africa the type of medicines he had spent his career producing.
The company was successful at establishing a high-quality production, but they found themselves competing against imports from countries, such as India and China, that were easy to buy and cheaper. There was little oversight of medicines that came into the African market to assure they were what they claimed to be.
Earlier this month, leaders from seven African nations met in Lomé, Togo to sign a political declaration to crack down on the trafficking of fake medicines in Africa, ratify existing international agreements, and introduce new criminal penalties against traffickers.
The U.K.-based Brazzaville Foundation organized the effort, known as the Lomé Initiative. The Foundation said it will establish an online site for the public to contribute additional ideas and solutions. Proposals that emerge from that process will be discussed at a follow-up forum in Africa before the end of the year.
“Today’s an important day, because it is the first time that us Africans are tackling the trafficking of fake medicines,” said H.E. Faure Gnassingbé, president of Togo during a plenary session of the high-level signing ceremony. “Our continent and our people suffer most from its devastating consequences. Africa must commit to fighting this deadly scourge.”
The problem of falsified medicine is a global problem with deadly consequences. The World Health Organization estimates 128 countries are affected by this problem.
It can be difficult to quantify the extent of the problem because falsified medicines that go undetected may lead a doctor to assume it was the wrong drug for the particular patient rather than the formulation or strength of the drug was different than the packaging claimed.
Each year, an estimated $200 billion of substandard and falsified drugs are sold, which is between 10 to 15 percent of the global pharmaceutical market, according to the World Health Organization. That comes with deadly consequences for the unsuspecting consumers of these falsified or substandard medicines. More than 122,000 children under five die each year due to poor-quality antimalarials in sub-Saharan Africa alone, according to estimates from the American Society of Tropical Medicine and Hygiene.
The problem is particularly acute in Africa, where some 42 percent of all falsified medicines discovered since 2013 have been found, according to the World Health Organization. It estimates that falsified medicines account for anywhere between 30 percent and 60 percent of all medicines sold in certain African countries. In contrast, countries that have established regulations and enforcement, this figure is is just 1 percent.
“These death traffickers do not know any borders,” said Aminata Touré, President of the Economic and Social Council of Senegal, who moderated the summit. “It is crucial that our countries work together, define intergovernmental cooperation mechanisms, share intel, and harmonize legislation to criminalize this activity.”
The Lomé Initiative is a positive step toward protecting and improving the health of Africans, but as my friend recently remarked to me in response to it, “Our leaders always meet but problem persists.”
His remark wasn’t intended to be cynical. It was meant to reflect the reality that Africans will continue to be susceptible to falsified medicines until we address the lack of capacity within the continent to produce the drugs its people need. They will remain vulnerable as long as Africa remains dependent on foreign companies to provide the medicines it requires to assure the health and wellbeing of its people.
To truly combat the problem of falsified medicine, Africa must do far more than criminalize the activity. It must work towards building capacity for its own pharmaceutical industry. To do so will require addressing a range of complex issues from access to capital to building needed infrastructure. It will also require establishing a world-class regulatory capacity operated by competent and empowered regulators to ensure the quality of medicines.
This is not just an urgent issue for the economic future of the continent, but a matter upon which the health and wellbeing of its people will depend.
Dr. Menghis Bairu is a physician, international biopharmaceutical executive, author, and philanthropist. He is founder, chairman, and CEO of Proxenia Venture Partners, which seeks to build companies that address global challenges through innovative approaches.
Dear friends:
I recently returned from Ethiopia and Eritrea where I had the opportunity to work with the Himalayan Cataract Project (HCP), a US based nonprofit that, in partnership with in-country stakeholders, seeks to eradicate preventable and curable blindness in underserved areas of the world. I wanted to share my recent experience with others who may be inspired to support efforts to restore sight and life to the needlessly blind in some of the most difficult to reach locations on the planet.
As a physician and life science executive, I’ve dedicated my professional life working to improve global health through international outreach and philanthropy. Though I live in the San Francisco Bay Area, I feel a deep commitment to giving back to my broader community of origin.
In November, I coordinated and worked with the HCP to conduct a high-volume surgical outreach and training event in Ethiopia and Eritrea. HCP performed 4,300 sight-restoring surgeries and clinical training in less than three week's time. The clinical team was from the United States, Nepal, Ethiopia and Eritrea. It represented a true international effort.
Since 1995, HCP has been providing the highest quality care at the lowest cost in its effort to end preventable blindness. There are 36 million people blind in the world today and nearly half of them—13.4 million people—are blind from cataracts. The organization has an innovative model to address both the huge backlog of people waiting for cataract surgery and the need to train more clinicians to do the work—each sight-restoring surgery performed takes ten minutes and costs $25 in materials.
The HCP has agreed to return to the region in early 2020 to perform 4,000 additional cataract surgeries. To enable this to happen, we need to raise $100,000 to fund the effort.
I've seen first-hand the immeasurable joy radiating from Ethiopians and Eritreans after having their sight restored by HCP, and a world of darkness is washed away with the careful touch of a surgeon. I support the Himalayan Cataract Project because we can solve needless blindness in our lifetime, but only if we work together. Please join in me supporting such a critical cause and donate today!
Sincerely,
Menghis Bairu, MD
About HCP | CureBlindness

Innovative Eye Care Model - HCP works to overcome barriers impeding delivery of cataract care to underserved, needlessly blind people.
Read more

At HCP’s first-ever surgical outreach in Eritrea, Dr. Menghis stood by a young boy's side in a difficult situation.
Read more

HCP co-founders Drs. Geoff Tabin and Sanduk Ruit, and their revolutionary, low-cost, 10-minute procedure caught the attention of 60 Minutes, ...
Watch the Story

Change lives with the gift of sight: join HCP's efforts to eradicate preventable blindness
https://charity.gofundme.com/o/en/campaign/giving-the-gift-of-sight-in-ethiopia-and-eritrea
The effects of blindness are profound and felt mostly by the poor. Lives are shortened, men and women are torn from the labor force, and kids are robbed of a childhood. In low- and middle-income countries, the effects of blindness have devastating consequences on these individuals and their families.
What makes this situation even more tragic is that 80 percent of blindness is treatable or preventable. In the developing world, 18 million people are unable to perform the tasks of daily living because of cataracts that can be addressed with a 10-minute surgery that requires just $25 in materials.
The Himalayan Cataract Project (HCP) works to cure preventable blindness. Since its establishment in 1995, HCP has been committed to overcoming barriers impeding delivery of cataract care to underserved, needlessly blind people in low- and middle-income countries with a focus on providing high-quality care, training local personnel, and establishing world-class eye care infrastructure where it is needed most. In 2019 alone, Dr Tilahun Kiros and his team conducted six campaigns in Tigray, Ethiopia for over 6,952 sight restoring surgeries.
| 2019 | Cataract Surgeries | TT Surgeries | Other Surgeries | Total Surgeries |
|---|---|---|---|---|
| Quiha | 3997 | 893 | 60 | 4950 |
| Axum | 1338 | 304 | 0 | 1642 |
We are working now to raise $100,000 to restore sight to 4,000 visually impaired patients in Eritrea and Ethiopia by March 31, 2020. You can help. I am asking that you consider making a $25 contribution to help our effort. Thanks to the generous support of people like you, we have raised $57,350 of $100,000 goal in just two weeks.
If you haven’t done so, please give the Gift of Sight now. If you have, thank you and please encourage others to do the same.

