SUBSCRIBE
For COVID-19 Related Questions: Email [email protected] or
ASK NOW!
For COVID-19 Related Questions: Email
[email protected] or
ASK NOW!
Latest on Cardiac Care
- Home
- Latest on Cardiac Care
Why do patients with acute hemorrhage become anemic?
By: Tweet by Dr Tony Breu @Tony_breau
I've spent way too much time recently thinking about this question. The explanation may seem obvious (if someone losses blood, they become anemic from, well, blood loss!), but the mechanism is far more interesting...
First, it's important to remember that hemoglobin is a concentration (grams per deciliter).

When someone bleeds, they bleed whole blood. The blood that is lost has the same concentration (hemoglobin) as the blood that is left behind (i.e., the blood that's still in the patient).
So, if you check a hemoglobin 5 minutes after a massive hemorrhage, what will you find? HGB IS UNCHANGED
The hemoglobin should be unchanged. They just bled blood that has the same concentration as what was left behind.
But they do become anemic, eventually. Why? Let's assume they aren't given liters of IVF. So, it there must be a fluid shift. Where does the fluid shift from? INTERSTITIAL SPACE
The shift can't be from the intravascular space because that's where we're hoping to shift fluid into.
It isn't the intracellular space either...
To understand why, think about what causes fluid to move out of a cell: an increase in ECF concentration. When you bleed whole blood, the ECF concentration does not change. There is no reason for fluid to move out of cells.
Instead, the fluid comes from the interstitium.
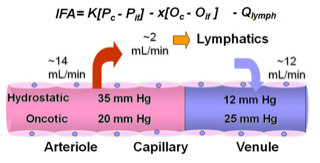
Why would fluid shift from the interstitium? Baroreceptors sense a drop in arterial and venous pressure leading to an increase in sympathetic tone. This increase in tone leads to arteriolar vasoconstriction leading to decreased capillary pressure.
When a patient has a decrease in capillary pressure, the Starling Equation suggests that fluid will move from the interstitial space into the vascular space. This, finally, is what leads to anemia. The plasma is "diluted" by fluid shifting from the interstitium.
If you're interested in reading more about the pathophysiologic response to acute blood loss (there is more!), I highly suggest:

